Introduction: Understanding Pain Perception
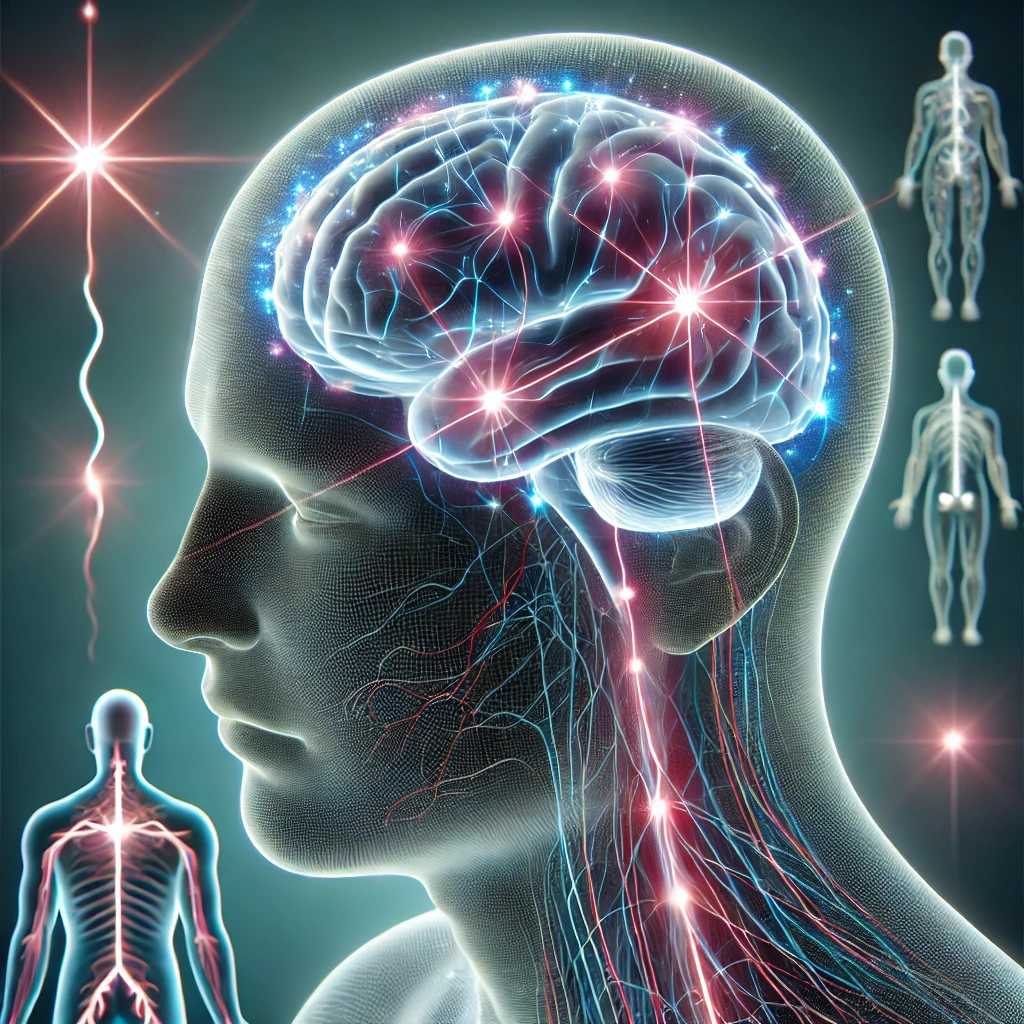
Pain perception in the brain is a highly complex and essential function of the nervous system. It acts as an internal alarm system, alerting us to potential injuries and prompting protective actions. Without the ability to perceive pain, even minor injuries could become life-threatening.
Pain is not merely a physical sensation; it is deeply intertwined with cognitive and emotional responses. The brain determines how intense pain feels, how long it lasts, and even whether it is perceived as tolerable or unbearable. This explains why two individuals may experience the same injury but report vastly different levels of discomfort.
In this article, we will explore the science of pain perception, how the brain processes pain signals, and the latest research on managing and altering pain perception.
The Science Behind Pain Perception
Pain perception begins when nociceptors (pain receptors) in the skin, muscles, and internal organs detect harmful stimuli, such as heat, pressure, or chemical irritation. These receptors send electrical signals through the nervous system, eventually reaching the brain.
Key Steps in Pain Processing
- Detection (Nociception)
- Sensory neurons recognize painful stimuli and send signals to the spinal cord.
- Specialized nociceptors respond to different pain types (thermal, mechanical, chemical).
- Transmission
- Signals travel along afferent nerve fibers toward the spinal cord.
- The dorsal horn of the spinal cord processes these signals before sending them to the brain.
- Perception
- The thalamus acts as a relay station, directing signals to various brain regions.
- The somatosensory cortex determines the location and intensity of pain.
- The limbic system processes the emotional response to pain.
- Modulation
- The brain can amplify or suppress pain signals based on cognitive and emotional factors.
- The periaqueductal gray (PAG) region releases endorphins to reduce pain.
Acute vs. Chronic Pain: What’s the Difference?
| Feature | Acute Pain | Chronic Pain |
|---|---|---|
| Cause | Injury, surgery, or temporary illness | Persistent conditions like arthritis or nerve damage |
| Duration | Short-term (hours to weeks) | Long-term (months to years) |
| Function | Protective (alerts body to danger) | Often maladaptive, serving no clear purpose |
| Treatment | Usually resolves with healing | Requires ongoing management strategies |
Why Does Pain Become Chronic?
When pain persists beyond the expected healing period, it may be due to neuroplastic changes in the brain. The nervous system can become hypersensitive, continuously transmitting pain signals even without actual tissue damage.
This is common in conditions like:
- Fibromyalgia (widespread pain without clear injury)
- Neuropathy (nerve damage-related pain)
- Complex Regional Pain Syndrome (CRPS) (intense pain from minor injuries)
Understanding how the brain “learns” pain is key to developing effective treatments.
How the Brain Modulates Pain Perception
Our brain does not simply receive pain signals—it actively modifies how we feel pain based on context, emotions, and past experiences.
Key Factors That Influence Pain Perception
- Expectation and Attention
- If you expect something to hurt, you will likely perceive more pain.
- Distraction techniques (e.g., music, VR therapy) can reduce pain intensity.
- Emotional State
- Anxiety and depression increase pain sensitivity.
- Positive emotions and mindfulness can lower pain perception.
- Placebo & Nocebo Effects
- Placebo Effect: Believing a treatment works can trigger pain relief.
- Nocebo Effect: Expecting pain can make it worse.
Neurotransmitters Involved in Pain Processing
| Neurotransmitter | Function in Pain |
|---|---|
| Glutamate | Excitatory; amplifies pain signals |
| Substance P | Enhances pain transmission |
| Endorphins | Natural painkillers that block pain signals |
| Serotonin & Dopamine | Influence mood and pain tolerance |
How to Train Your Brain to Reduce Pain
Since the brain actively shapes our pain experience, modifying neural pathways can help manage pain effectively.
1. Mindfulness Meditation
- Studies show meditation reduces activity in the pain-processing regions of the brain.
- Long-term practice increases gray matter density in areas associated with pain modulation.
2. Cognitive Behavioral Therapy (CBT)
- Helps patients reframe negative thoughts about pain.
- Reduces catastrophizing, which can amplify pain perception.
3. Physical Activity & Exercise
- Releases endorphins, which are natural pain relievers.
- Strengthens muscles, reducing mechanical strain and discomfort.
4. Diet & Nutrition
- Anti-inflammatory foods (e.g., turmeric, omega-3s) can reduce chronic pain.
- Magnesium-rich foods help relax muscles and nerves.
Cutting-Edge Pain Research: What’s Next?
- Virtual Reality (VR) Pain Therapy
- Immersive VR environments distract the brain, reducing pain perception.
- Gene Therapy for Chronic Pain
- Targeting specific pain-related genes could provide long-term relief.
- Neurostimulation Devices
- Brain implants and spinal cord stimulators block pain signals at the source.
Conclusion: The Future of Pain Management
Pain perception in the brain is a highly dynamic process influenced by biology, psychology, and environment. While pain is essential for survival, chronic pain can be debilitating. Fortunately, advancements in neuroscience, mindfulness, and personalized medicine are paving the way for better pain management strategies.
By understanding how the brain interprets pain, we can develop more effective treatments and improve quality of life for those suffering from chronic pain conditions.
